Hoffa’s Fat Pad (HFP)
What is Hoffa’s fat pad?
Hoffa’s fat pad (infrapatellar) is a pad of fatty tissue which lies under the knee cap in-between the joint capsule and synovium. Hoffa’s fat pad is a small pocket of fat which sits just below the knee joint to protect the patella tendon, patella and bone surfaces from the movement of the tibia and femur bones. The fat pad can become inflamed and swell in a horseshoe like shape which may cause pain in the front on the knee.
Pain is communally felt over the site of swelling but can be felt on either side or more to one side. This can occur due to the fat pad becoming irritated or impinged due to a number of reasons, some including direct trauma or hip and knee alignment. Irritation may also occur as a secondary cause when dealing with meniscus or ligament damage/disorders.
Pain is exacerbated by extending the knee, wearing high heels, kicking, climbing stairs or squatting for long periods of time. It is common to experience pain at the front of the knee, just below the kneecap, however other conditions including patellofemoral pain and patellar tendonitis have the same symptoms so visit a physiotherapist for a full examination. In younger patients 10-14 years old Osgood-Schlatter causes swelling of the cartilage, patella tendon and the bursa’s. This can contribute to young athletes suffering from Hoffa’s fat pad pain in the front of their knee.

What causes Hoffa’s fat pad?
Fat pad impingement can be caused by:
- Tight quadriceps
- Anterior pelvic tilt
- Direct impact to the knee
- Scarring and hardening of the fat pad
- Hip or knee alignment
- Osteoarthritis
- Extreme extension of the knee (Genu Recurvatum)
Who’s more likely to suffer from Hoffa’s fat pad?
- People who are involved in sports where direct contact to the knee can occur (hockey, football, rugby and martial arts
- ACL injury due to reduced stability in the knee
- Hypermobility
- Hyperextension of the knee
- Iliotibial band syndrome
- Runners who have flat feet due to muscle weakness/imbalance
How can you treat Hoffa’s fat pad?
Knee pain treatments include:
- Cold therapy to bring down swelling or inflammation
- Massage on the Quadriceps to reduce tightness in the muscle
- Rest and avoid activities that strain the knee
- Electrotherapy (TENS or ultrasound)
- Exercises the strengthen the knee
- Anti-inflammatory drugs
- K tape to offload the knee putting less strain on it
- Steroid injections – only in serious cases
How cold therapy helps Hoffa’s fat pad
Local cryotherapy can help to reduce pain, swelling and inflammation for both acute and chronic injuries. The cold air applied to the skin triggers the body’s anti-inflammatory responses. This is due to the cold air creating an immediate rush of oxygenated blood to the area of treatment which will cause a reduction of tension in the muscle. The use of localised cryotherapy has been found to have beneficial effects on oedema, pain, reduction in bleeding, haematomas and inflammation (Rana, M. et al., 2011).
How can Kinesio Tape (K Tape) help Hoffa’s Fat Pad?
K Taping can help to elevate pressure of the knee cap on the fat pad. This tape can be applied in many ways and you should find a way that works best for you to offer pain relief. The tape is normally applied under the patella in a V shape lifting the soft tissue up to offload the fat pad. This has been found to help settle symptoms while also allowing range of motion so patients can participate in activities/sports relatively pain free (Dragoo, J.L., Johnson, C. and McConnell, J., 2012)
Polymyalgia Rheumatica (PMR)
What is PMR?
Polymyalgia Rheumatica (PMR) is an inflammatory disease which causes pain, stiffness and inflammation in the muscles around the shoulders, neck and hips. PMR is more common in women, typically develops between the ages of 50 and 70. The main symptom is muscle stiffness in the morning lasting longer than 45 minutes. Diagnosing PMR is very difficult as the symptoms are similar to rheumatoid arthritis. This needs to be ruled out before PMR is diagnosed. There is also a close link to a condition called giant cell arteritis (GCA) which is a type of blood vessel inflammation. Symptoms for GCA include headache, jaw pain and vision changes. This only affect 10% of patients with PMR.

Symptoms of PMR:
- Morning muscle stiffness
- Extreme tiredness
- Weight loss
- Depression
What causes PMR?
The cause of PMR is inflammation, however it is unknown what causes the inflammation. It is an age related condition which most people are over the age of 65 and is more common in women. Causes are normally a combination of genetic and environmental factors.
How can you treat PMR?
PMR is normally treated with steroid medicine called prednisolone. Most people require a course of treatment which lasts from 12 months to 2 years to prevent symptoms returning.
Prednisolone
Prednisolone works by blocking the effects of a chemical which causes inflammation in the body. This does not cure PMR but it can help to relieve symptoms. Most people will take several tablets once a day which will then be gradually reduced every couple of months, however you may need to take the tablets for 1-2 years. PMR often gets better by itself however it can come back after treatment.
Cryotherapy
Full body cryotherapy increases the amount of white blood cells in your body which is part of the immune system. This triggers an immune response which decreases inflammation by increasing the number of anti-inflammatory cytokines. As PMR is an inflammatory disease whole body cryotherapy can help to reduce symptoms if clients don’t want to take steroids or unfortunately if the steroids are not working.
Cryotherapy has been proven to reduce the arthritis score in patients as well as localised cryotherapy showing a beneficial response in reducing inflammation in joints. (Peyronnel, C et al., 2022)
De Quervain’s Tenosynovitis
What is De Quervain’s Tenosynovitis?
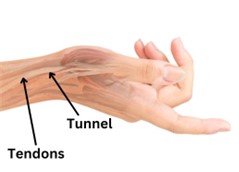
De Quervain’s tenosynovitis is a condition that affects the tendons in the wrist which affects the tunnel on the thumb side of the wrist. This conditions occurs when the tendons are constricted by the sheath which runs from the wrist to the hand.
The exact cause of De Quervain’s tenosynovitis isn’t known but activities than rely on wrist movements especially repetitive movements e.g. gardening, gold etc. can make it worse.
What causes De Quervain’s Tenosynovitis?
De Quervain’s is causes by irritation of the tendons in the thumb (extensor pollicis brevis and abductor pollicis longus). The tendon becomes thicken and narrowed which causes inflammation and pain when moving your wrist and thumb.
- There normally isn’t an obvious cause but symptoms are aggravated after prolonged or unusual activities e.g. gardening, gaming or sports.
- It is more common in women who have just had a baby due to the hormonal changes or repetitive lifting of the baby. However, which of these is the cause is unclear.
- People with rheumatoid arthritis may be more susceptible
- It is more common in women than men
- It is more common in people aged 40-50
What are the symptoms?
- Pain is normally felt in the wrist on the thumb side. This is aggravated by lifting the thumb especially when using scissors
- Tenderness is normally felt on the site of pain
- Swelling in the wrist
- Clicking or snapping of the tendons may occasionally occur
How can you treat De Quervain’s Tenosynovitis?
- Splints
- Anti-inflammatory drugs
- Avoid activities that cause pain
- Corticosteroids injections
- Cold therapy to bring down swelling or inflammation
- Surgical decompression
50% – 80% of cases can be successfully treated non-surgically with splints, NSAIDs and injections.
Cryotherapy
Local cryotherapy can help to reduce, pain, swelling and inflammation. The cold air triggers a rush of blood to area of treatment which triggers anti-inflammatory responses within the body. Cryogenic temperatures have been found to improve overall well-being (relaxation), creates an analgesic effect, increases systemic immunity (Lubkowska, A., 2012).





